Blood is often called the “river of life” because it carries oxygen, nutrients, and essential components to every cell in our body. But what happens when this very lifeline is disrupted at its core—inside the bone marrow where blood cells are formed? This is where blood cancer comes into the picture. Blood cancer, though frightening to hear, is not a single disease but rather a group of cancers that affect how blood cells are produced, function, and grow.
This guide will walk you through everything you need to know about blood cancer—what it is, its types, causes, symptoms, risk factors, treatments, and how people cope with it. Whether you’re a patient, caregiver, or someone seeking awareness, this comprehensive guide aims to bring clarity and hope.
What is Blood Cancer?
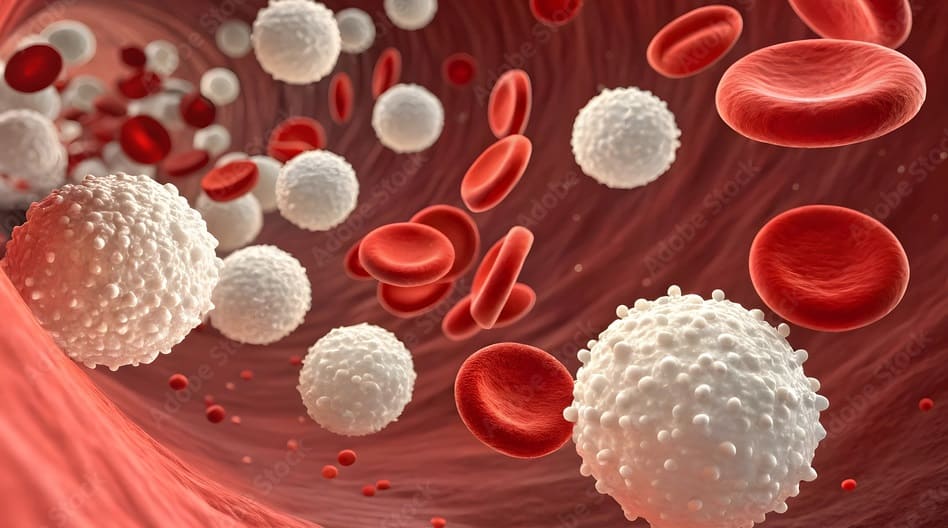
Blood cancer, also known as hematologic cancer, begins in the bone marrow—the spongy tissue inside bones where blood cells are made. Normally, blood stem cells develop into red blood cells (which carry oxygen), white blood cells (which fight infections), and platelets (which help in clotting).
In blood cancer, this process goes wrong. Abnormal blood cells grow uncontrollably and interfere with the body’s ability to function properly. These abnormal cells can crowd out healthy blood cells, weaken the immune system, and disrupt the body’s ability to transport oxygen, fight infections, and prevent bleeding.
Types of Blood Cancer
Blood cancers are broadly categorized into three main types:
1. Leukemia
Leukemia begins in the bone marrow and results in the production of abnormal white blood cells. These cells do not function properly and multiply rapidly, crowding out healthy cells. Leukemia is further classified as:
- Acute Lymphoblastic Leukemia (ALL): Most common in children but can affect adults. Progresses quickly.
- Acute Myeloid Leukemia (AML): Common in adults; progresses rapidly.
- Chronic Lymphocytic Leukemia (CLL): Progresses slowly; usually affects older adults.
- Chronic Myeloid Leukemia (CML): Affects adults; progresses slowly at first but can become aggressive.
2. Lymphoma
Lymphoma affects the lymphatic system, which is part of the immune system. It occurs when lymphocytes (a type of white blood cell) become abnormal and multiply uncontrollably.
- Hodgkin Lymphoma (HL): Characterized by the presence of Reed-Sternberg cells. It is highly treatable.
- Non-Hodgkin Lymphoma (NHL): More common and includes many subtypes, ranging from slow-growing to aggressive forms.
3. Myeloma
Also called multiple myeloma, this cancer begins in plasma cells, a type of white blood cell responsible for producing antibodies. Cancerous plasma cells accumulate in the bone marrow and interfere with the production of normal blood cells.
Symptoms of Blood Cancer
Blood cancer symptoms can vary depending on the type, but common warning signs include:
- Persistent fatigue or weakness
- Fever and chills
- Frequent infections
- Unexplained weight loss
- Swollen lymph nodes (especially in the neck, armpits, or groin)
- Night sweats
- Easy bruising or bleeding (such as nosebleeds, bleeding gums, or small red spots on the skin)
- Bone or joint pain
- Shortness of breath
- Enlarged spleen or liver
It’s important to note that these symptoms are not exclusive to blood cancer. However, if they persist or worsen, consulting a doctor is essential.
Causes and Risk Factors
The exact cause of blood cancer is not fully understood, but several factors may increase the risk:
1. Genetic Factors:
- Family history of blood cancers
- Inherited genetic mutations (e.g., Down syndrome)
2. Environmental Exposure:
- Long-term exposure to radiation
- Harmful chemicals such as benzene
3. Weakened Immune System:
- HIV/AIDS or other immune deficiencies
- Organ transplant patients on immunosuppressive drugs
4. Age and Gender:
- Certain types like CLL and AML are more common in older adults.
- Men are slightly more likely than women to develop some blood cancers.
5. Previous Cancer Treatments:
- Chemotherapy or radiation therapy for other cancers can sometimes increase the risk of blood cancers later in life.
How is Blood Cancer Diagnosed?
Early detection is key to better outcomes. Doctors use a combination of tests to diagnose blood cancer:
- Physical Examination: Checking for swollen lymph nodes, enlarged liver, or spleen.
- Blood Tests: Complete blood count (CBC) to look for abnormal levels of red cells, white cells, or platelets.
- Bone Marrow Biopsy: Extracting a sample from bone marrow to detect abnormal cells.
- Imaging Tests: X-rays, CT scans, PET scans, or MRIs to check for organ or lymph node involvement.
- Genetic and Molecular Testing: Identifying specific mutations that may guide treatment.
Stages of Blood Cancer
Unlike solid tumors, staging in blood cancers is more complex. It depends on the type of cancer and extent of spread:
- Leukemia: Classified by cell type (myeloid or lymphoid) and progression (acute or chronic).
- Lymphoma: Staged I to IV based on how many lymph nodes and regions are affected.
- Myeloma: Staged based on the level of abnormal proteins in blood and bone damage.
Treatments for Blood Cancer
Treatment depends on the type of blood cancer, stage, age, and overall health of the patient. Common approaches include:
1. Chemotherapy
Uses strong drugs to kill or stop the growth of cancer cells. Can be given orally or intravenously.
2. Radiation Therapy
Uses high-energy rays to target and destroy cancer cells, often used for lymphoma or localized bone lesions.
3. Targeted Therapy
Focuses on specific genes, proteins, or pathways that cancer cells use to grow. For example, tyrosine kinase inhibitors in CML.
4. Immunotherapy
Boosts the body’s immune system to fight cancer. This includes monoclonal antibodies and CAR-T cell therapy.
5. Stem Cell Transplant (Bone Marrow Transplant)
Replaces diseased bone marrow with healthy stem cells, either from the patient (autologous) or a donor (allogeneic).
6. Supportive Care
Blood transfusions, antibiotics, and medications to reduce symptoms and improve quality of life.
Living with Blood Cancer
A diagnosis of blood cancer can be overwhelming, but advances in medical research have improved survival rates significantly. Living with blood cancer involves:
- Regular Monitoring: Frequent blood tests and follow-ups.
- Diet and Nutrition: Eating a balanced diet to support immunity.
- Mental Health Support: Counseling, support groups, and therapy help patients cope emotionally.
- Managing Side Effects: Fatigue, nausea, infections, and hair loss are common but manageable with medical guidance.
How to Prevent Blood Cancer
While blood cancer cannot always be prevented, certain steps can help reduce risk:
- Limiting exposure to harmful chemicals
- Avoiding unnecessary radiation exposure
- Maintaining a strong immune system through healthy lifestyle choices
- Regular health check-ups, especially for those with a family history of blood cancer
Prognosis and Survival Rates
Survival rates vary widely depending on the type and stage of blood cancer:
- Leukemia: Five-year survival rates range from 40% to over 80% depending on type.
- Lymphoma: Hodgkin lymphoma has a survival rate of over 85%, while non-Hodgkin lymphoma varies.
- Myeloma: Treatments have improved survival, with many patients living 5–10 years or more after diagnosis.
Research and Advances in Blood Cancer Treatment
Medical research is continuously evolving. Some breakthroughs include:
- CAR-T cell therapy for resistant leukemias and lymphomas.
- New targeted drugs such as kinase inhibitors.
- Precision medicine, where treatments are tailored based on genetic mutations.
- Advances in stem cell transplantation with reduced complications.
These advancements bring new hope to patients and families facing blood cancer.
Coping as a Patient or Caregiver
Blood cancer not only affects the patient but also their family and caregivers. Here are some coping strategies:
- Education: Learn as much as possible about the disease.
- Support Groups: Connect with others going through similar experiences.
- Stress Management: Yoga, meditation, and relaxation techniques can help.
- Financial Planning: Explore insurance and support programs for treatment costs.
Conclusion
Blood cancer is a complex and life-changing condition, but it is no longer the hopeless diagnosis it once was. Advances in medical science, better diagnostic tools, and innovative therapies have transformed survival and quality of life for many patients. Awareness, early detection, and timely treatment remain the most powerful tools in the fight against blood cancer. If you or a loved one has been diagnosed, remember—you are not alone. With the right medical support, emotional care, and treatment options, there is always hope.
FAQ’s
Is blood cancer curable?
Some types, such as Hodgkin lymphoma and certain cases of acute lymphoblastic leukemia, can be cured. Other types may not be fully curable but can be managed effectively with long-term treatment.
Who is at risk of developing blood cancer?
Older adults, people with weakened immune systems, those with family history, and individuals exposed to radiation or harmful chemicals are at higher risk.
Can children get blood cancer?
Yes, leukemia is the most common type of childhood cancer, but survival rates in children are often very high with modern treatment.
Does blood cancer spread quickly?
It depends on the type. Acute leukemias progress rapidly, while chronic leukemias and some lymphomas may develop slowly over time.
Can blood cancer come back after treatment?
Yes, relapse can occur. However, second-line therapies, targeted treatments, and stem cell transplants offer hope for remission.
What lifestyle changes help blood cancer patients?
A balanced diet, adequate rest, infection prevention, stress management, and regular medical follow-ups can improve quality of life.
What is the survival rate of blood cancer?
Survival depends on the type and stage. Hodgkin lymphoma has survival rates above 85%, while other types like acute leukemia and myeloma vary based on patient factors and treatment response.
Is blood cancer hereditary?
While most cases are not directly inherited, family history may slightly increase risk.
Can lifestyle changes reduce the risk of blood cancer?
Yes, avoiding harmful chemicals, radiation exposure, and maintaining overall health may lower risk, but not all cases are preventable.
What is the life expectancy of someone with blood cancer?
It varies widely by type and stage. Some patients live decades with proper treatment, while others may face more aggressive disease.
How is blood cancer different from other cancers?
Blood cancer originates in bone marrow and blood cells, not solid tumors, which makes staging and treatment unique.
How long can a person live with cancer in the blood?
Life expectancy depends on the type of blood cancer, stage at diagnosis, age, and overall health. Some people with chronic leukemias can live for decades with treatment, while aggressive forms like acute leukemia may require immediate therapy but can still achieve remission. Advances in targeted therapies and stem cell transplants have significantly improved survival rates.
What is the last stage of blood cancer?
In the final stage, blood cancer has usually spread widely—affecting bone marrow, blood, lymph nodes, and sometimes organs like the liver, spleen, or lungs. Patients may experience severe fatigue, frequent infections, bleeding, weight loss, and difficulty breathing. At this stage, treatment often focuses on symptom management and improving quality of life, although some therapies may still help control the disease.
Also Read: