When we think about chronic diseases, we often categorize them separately—heart disease in one box, kidney problems in another, and metabolic issues like diabetes and obesity in yet another. But the truth is, these conditions are not isolated. They are deeply connected, often overlapping, and when they do, they create a dangerous cycle that significantly increases the risk of early death. This interconnected web of conditions is now recognized under a unified name: Cardiovascular-Kidney-Metabolic (CKM) Syndrome.
This recognition is more than just a new medical label—it’s a wake-up call for patients, doctors, and public health systems. Understanding CKM Syndrome allows us to detect risks earlier, manage patients more holistically, and hopefully prevent devastating outcomes like heart attacks, kidney failure, or premature death. In this guide, we’ll dive deep into what CKM Syndrome is, why it matters, how it develops, its stages, risk factors, symptoms, diagnosis, treatment approaches, and lifestyle strategies for prevention. Let’s begin.
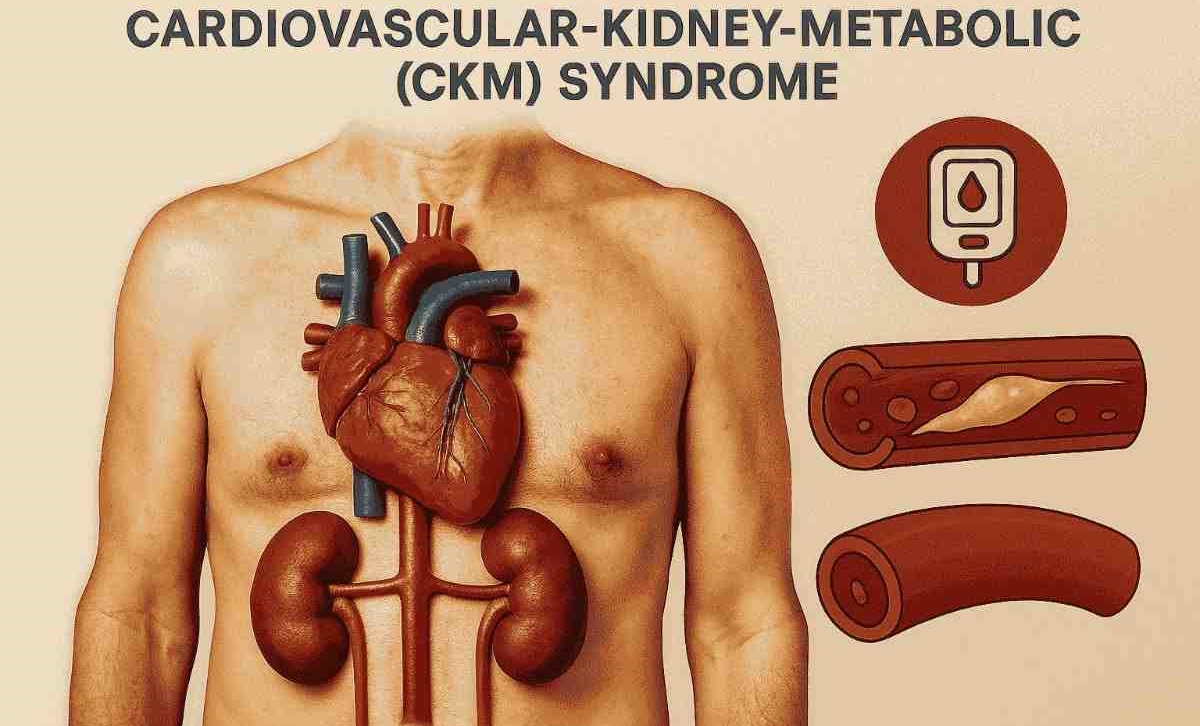
What is Cardiovascular-Kidney-Metabolic (CKM) Syndrome?
Cardiovascular-Kidney-Metabolic (CKM) Syndrome is a medical term used to describe the interconnected health conditions involving the heart (cardiovascular), kidneys (renal), and metabolism (including diabetes, obesity, and insulin resistance).
Rather than treating each disease separately, CKM recognizes that these conditions are interdependent and often feed into one another. For example:
- Diabetes can damage blood vessels, increasing the risk of heart disease.
- High blood pressure can strain the kidneys and lead to chronic kidney disease.
- Kidney dysfunction can further elevate heart risks and worsen metabolic imbalance.
The American Heart Association (AHA) formally introduced the CKM Syndrome framework in 2023 to encourage integrated care and earlier risk detection. This step acknowledges that if we only focus on one organ or disease, we miss the bigger picture of how these conditions accelerate one another.
Why Does CKM Syndrome Matter?
CKM Syndrome is not just a medical concept—it has life-changing implications. Here’s why it matters:
- High prevalence: Millions of people worldwide live with diabetes, obesity, kidney disease, or heart conditions. Many of them have more than one at the same time.
- Early death risk: People with overlapping CKM conditions face a much higher risk of premature death compared to those with isolated issues.
- Healthcare burden: CKM contributes significantly to hospitalizations, dialysis needs, surgeries, and medication dependence.
- Silent progression: The syndrome often develops silently for years before showing severe symptoms.
By grouping these conditions together, CKM Syndrome pushes doctors and patients to take a proactive, holistic approach to health.
Stages of CKM Syndrome
The AHA framework divides CKM Syndrome into five stages, from early risk to advanced disease:
- Stage 0 – No current risk: Individuals with no known risk factors for cardiovascular, kidney, or metabolic conditions.
- Stage 1 – Increased risk: People with lifestyle risks such as obesity, family history, or poor diet, but without established disease.
- Stage 2 – Early disease: Presence of metabolic risk factors like prediabetes, hypertension, high cholesterol, or mild kidney dysfunction.
- Stage 3 – Established disease: Diagnosed type 2 diabetes, moderate-to-severe chronic kidney disease, or clinical cardiovascular disease.
- Stage 4 – Advanced disease: Coexisting advanced heart disease, kidney failure, and severe metabolic imbalance, often leading to high risk of disability or death.
This staging system helps doctors identify where a patient falls on the spectrum and intervene before progression.
Causes and Risk Factors of CKM Syndrome
CKM Syndrome doesn’t appear overnight. It develops through a mix of genetic, lifestyle, and environmental factors. Common Risk Factors:
- Obesity: Especially abdominal obesity, which promotes insulin resistance.
- Type 2 diabetes or prediabetes: Major contributors to CKM progression.
- Hypertension (high blood pressure): Damages both heart and kidneys.
- High cholesterol: Increases cardiovascular burden.
- Chronic kidney disease (CKD): Even mild kidney impairment raises heart risks.
- Smoking and alcohol consumption: Both accelerate cardiovascular and metabolic damage.
- Sedentary lifestyle: Lack of physical activity worsens obesity and insulin resistance.
- Unhealthy diet: High in processed foods, sugar, and salt.
- Family history: Genetic predisposition plays a role.
- Chronic stress: Promotes hormonal imbalances that worsen metabolic health.
Symptoms of CKM Syndrome
Because CKM Syndrome involves multiple organ systems, symptoms may vary. Early stages often have no obvious signs, which makes screening critical. Possible Symptoms:
- Fatigue or weakness
- Frequent urination or thirst (suggestive of diabetes)
- Swelling in feet or ankles (kidney dysfunction or heart failure)
- Chest pain, palpitations, or shortness of breath (heart disease)
- Unexplained weight gain (fluid retention due to kidney or heart failure)
- Vision problems (linked to diabetes)
The challenge is that many people dismiss these as signs of aging or stress until the disease is advanced.
Diagnosis of CKM Syndrome
Diagnosing CKM Syndrome requires a multi-disciplinary approach since it involves heart, kidney, and metabolic health. Doctors may use:
- Medical history and family history assessment.
- Blood tests: Blood glucose, HbA1c (for diabetes), kidney function tests (creatinine, eGFR), lipid profile.
- Urine tests: Checking for protein or albumin (early kidney damage).
- Blood pressure monitoring.
- Body mass index (BMI) and waist circumference.
- Electrocardiogram (ECG) and echocardiography for heart function.
- Imaging tests (like ultrasound of kidneys or heart scans, if needed).
A comprehensive evaluation helps identify risk at earlier stages.
Management and Treatment of CKM Syndrome
Since CKM Syndrome involves multiple systems, treatment is not one-size-fits-all. Instead, it requires an integrated care plan targeting all three components:
1. Lifestyle Modifications
- Healthy diet: Focus on whole foods, fruits, vegetables, lean proteins, whole grains, and low sodium.
- Regular exercise: At least 150 minutes of moderate physical activity per week.
- Weight management: Achieving and maintaining a healthy weight can dramatically reduce risk.
- Quit smoking and limit alcohol.
- Stress management: Yoga, meditation, or mindfulness.
2. Medications
Depending on the patient’s conditions:
- Diabetes management: Insulin, metformin, or newer drugs like SGLT2 inhibitors and GLP-1 receptor agonists.
- Blood pressure control: ACE inhibitors, ARBs, or beta-blockers.
- Cholesterol-lowering drugs: Statins or PCSK9 inhibitors.
- Kidney protection drugs: SGLT2 inhibitors also benefit kidney health.
- Antiplatelets or anticoagulants: For cardiovascular protection in high-risk patients.
3. Regular Monitoring
- Routine blood sugar checks.
- Kidney function testing every few months.
- Heart evaluations if symptoms appear.
4. Coordinated Care
Ideally, patients with CKM Syndrome are managed by a multidisciplinary team including cardiologists, nephrologists, endocrinologists, dietitians, and primary care physicians.
How to Prevent CKM Syndrome?
Prevention is always better than treatment, especially with CKM Syndrome, where complications are often irreversible. Some prevention strategies include:
- Eat a heart- and kidney-friendly diet: Low in processed foods, sugars, and saturated fats.
- Stay active: Walking, swimming, or cycling can improve both metabolic and heart health.
- Check blood sugar and blood pressure regularly.
- Stay hydrated but avoid excess salt.
- Get regular health checkups, especially if you have a family history.
- Prioritize sleep and stress reduction.
The Global Impact of CKM Syndrome
CKM Syndrome isn’t just a medical issue—it’s a public health crisis. The World Health Organization (WHO) has long warned about the rising burden of non-communicable diseases like diabetes, obesity, and heart disease. With CKM, we now see how intertwined they are.
- Diabetes prevalence: Over 500 million people worldwide live with diabetes, and the number is expected to rise sharply.
- Kidney disease: Chronic kidney disease affects nearly 10% of the global population.
- Heart disease: The leading cause of death globally.
By addressing CKM Syndrome as a combined condition, healthcare systems can improve screening programs, reduce long-term healthcare costs, and save lives.
Living with CKM Syndrome: Patient Perspective
Being diagnosed with CKM Syndrome can feel overwhelming. Many patients struggle with the idea of managing multiple conditions at once. But with the right support, it is possible to live a full life.
- Education is key: Understanding how heart, kidney, and metabolism interact helps patients stay motivated.
- Small changes matter: Even modest weight loss or improved blood sugar control can dramatically reduce risks.
- Community and support groups: Sharing experiences helps reduce isolation.
Patients often find that once they adopt lifestyle changes for one condition (like diabetes), it benefits the others too. That’s the advantage of approaching CKM holistically.
Future of CKM Care
Medical research is moving rapidly toward better understanding CKM Syndrome. Exciting developments include:
- Precision medicine: Tailoring treatments based on genetics and individual health profiles.
- New drug therapies: SGLT2 inhibitors and GLP-1 agonists are already showing promise in protecting both heart and kidney health.
- AI and digital health: Wearables and apps to monitor glucose, heart rate, and kidney function in real-time.
- Integrated clinics: Centers where cardiology, nephrology, and endocrinology work together under one roof.
These advances hold hope for reducing the devastating impact of CKM in the coming decades.
Conclusion
Cardiovascular-Kidney-Metabolic (CKM) Syndrome represents a powerful shift in how we think about chronic diseases. Instead of treating the heart, kidneys, and metabolism separately, CKM recognizes their interconnected nature. By identifying risks earlier, encouraging lifestyle changes, and applying integrated medical care, we can prevent countless cases of premature death and disability.
If you’re at risk—or already living with diabetes, high blood pressure, kidney disease, or heart disease—the best step you can take today is to talk to your doctor about CKM risk. With awareness, prevention, and proactive care, CKM Syndrome doesn’t have to define your future.
FAQ’s
Is CKM Syndrome reversible?
In the early stages, CKM Syndrome can often be managed and in some cases reversed through lifestyle changes like eating a balanced diet, exercising regularly, and following medical advice. However, once advanced damage occurs—such as kidney failure or severe heart disease—it cannot be fully reversed. At that stage, treatment mainly focuses on slowing the progression, reducing complications, and improving quality of life.
Can CKM Syndrome lead to early death?
Yes, CKM Syndrome significantly increases the risk of heart attacks, strokes, kidney failure, and other life-threatening complications. This makes it one of the most concerning health conditions globally. The overlapping damage to the heart, kidneys, and metabolism creates a dangerous cycle that shortens lifespan if not detected and treated early.
What is the role of diet in CKM management?
Diet is one of the most powerful tools in managing CKM Syndrome. Choosing foods that protect the heart and kidneys while supporting healthy metabolism can slow disease progression. A balanced diet that includes fiber-rich foods, healthy fats, and controlled protein intake, along with limited processed foods and sodium, helps control blood pressure, blood sugar, and cholesterol. This not only reduces complications but also supports overall health and well-being.
What treatments are available for CKM Syndrome?
Treatment depends on the stage and severity of the syndrome. Doctors often prescribe medications to control blood sugar, blood pressure, and cholesterol. Newer drug classes such as SGLT2 inhibitors and GLP-1 receptor agonists have shown benefits for both heart and kidney protection. Lifestyle changes remain central to treatment, including diet, exercise, and weight management. In advanced stages, dialysis or surgery may be required to manage complications.
Can someone live a normal life with CKM Syndrome?
Yes, it is possible to live a fulfilling life with CKM Syndrome, especially when the condition is managed well. Early detection, consistent treatment, and healthy lifestyle changes can significantly reduce risks and improve day-to-day living. Many people find that adopting habits such as eating well, staying active, and following medical guidance not only help them manage CKM but also improve their overall quality of life.
Is CKM Syndrome the same as metabolic syndrome?
No, CKM Syndrome and metabolic syndrome are not the same, although they are related. Metabolic syndrome refers to a group of conditions—such as high blood sugar, high blood pressure, excess belly fat, and abnormal cholesterol levels—that increase the risk of heart disease and diabetes. CKM Syndrome goes beyond this by linking metabolic problems with kidney disease and cardiovascular disease under one framework. In other words, metabolic syndrome can be part of CKM, but CKM encompasses a broader and more integrated view of health.
Can children or young adults develop CKM Syndrome?
Yes, CKM Syndrome can affect younger people, especially those with obesity, type 2 diabetes, or a strong family history of heart or kidney disease. With rising childhood obesity rates, more adolescents are developing early signs of metabolic problems such as insulin resistance or high blood pressure. While full CKM Syndrome usually appears later in life, the foundation often starts in childhood or young adulthood, making early lifestyle interventions critical.
How fast does CKM Syndrome progress?
The speed of progression varies widely from person to person. Some individuals may live with early risk factors for years without major complications, while others may develop rapid worsening of kidney or heart function. Factors such as poor diet, uncontrolled diabetes, smoking, lack of exercise, and genetic predisposition accelerate the progression. Regular monitoring helps catch progression early so that treatment can slow it down.
How does stress affect CKM Syndrome?
Chronic stress has a strong impact on CKM Syndrome because it triggers hormonal imbalances that raise blood sugar, blood pressure, and inflammation in the body. Over time, this adds to the strain on the heart and kidneys while worsening metabolic health. Stress also leads to unhealthy coping habits like overeating, poor sleep, or smoking, which further fuel CKM progression. Managing stress through meditation, deep breathing, exercise, or counseling is a vital part of prevention and management.
What role does genetics play in CKM Syndrome?
Genetics can make some individuals more susceptible to CKM Syndrome. For example, a family history of diabetes, kidney disease, or heart disease increases the likelihood of developing these interconnected problems. However, genes are not destiny. Lifestyle choices such as diet, exercise, and avoiding smoking play a major role in whether those genetic risks turn into actual disease.
What tests should I ask my doctor for if I’m worried about CKM Syndrome?
If you are concerned about CKM Syndrome, ask your doctor for a comprehensive health checkup. This usually includes fasting blood sugar or HbA1c to check for diabetes, cholesterol and triglyceride levels, blood pressure monitoring, kidney function tests such as serum creatinine and eGFR, and urine tests for protein leakage. Depending on your age and risk profile, your doctor may also suggest heart evaluations such as an ECG or echocardiogram.
Can CKM Syndrome affect mental health?
Yes, living with CKM Syndrome can affect mental well-being. The stress of managing multiple health conditions, dietary restrictions, frequent doctor visits, and the fear of complications often contribute to anxiety and depression. Additionally, biological factors such as poor circulation or hormonal imbalance caused by CKM can also influence brain health. Integrating mental health support into treatment plans is essential for patients to maintain resilience and motivation.
Does CKM Syndrome affect men and women differently?
Both men and women are at risk, but the patterns can differ. Men are generally more prone to earlier heart disease, while women with diabetes have a disproportionately higher risk of cardiovascular problems compared to men with diabetes. Hormonal differences, body fat distribution, and post-menopausal changes also influence CKM risk in women. Understanding these differences helps doctors tailor prevention and treatment more effectively.
Can CKM Syndrome be prevented completely?
While not every case of CKM Syndrome can be prevented, especially for people with strong genetic risk factors, the majority of cases can be delayed or reduced in severity through lifestyle changes. Maintaining a healthy weight, staying physically active, avoiding smoking, eating a balanced diet, and managing stress significantly lower the chances of developing CKM. Regular screenings help catch early signs before the condition advances.
What is the long-term outlook for people with CKM Syndrome?
The long-term outlook depends on how early the condition is detected and how consistently it is managed. People who make lifestyle changes, take medications as prescribed, and regularly monitor their health can slow the disease and live long, fulfilling lives. On the other hand, untreated CKM Syndrome often leads to kidney failure, severe heart disease, or stroke, which can shorten lifespan. Awareness, prevention, and holistic management are key to improving outcomes.
Also Read: