Pregnancy is often painted as a beautiful, glowing journey filled with tiny kicks, gentle cravings, and dreams of holding a newborn. But for some women, this journey takes an unexpected and frightening turn. One such serious and often misunderstood complication is HELLP Syndrome.
Unlike morning sickness or swollen feet, HELLP Syndrome does not always come with loud warning signs. It can creep in quietly, masquerading as normal pregnancy discomforts, and progress rapidly into a life-threatening emergency for both mother and baby. Many women have never even heard of it until they are diagnosed with it.
This guide is written not just to inform, but to support, reassure, and prepare you. Because awareness is power, especially when it comes to something as serious as HELLP Syndrome.
What is HELLP Syndrome?
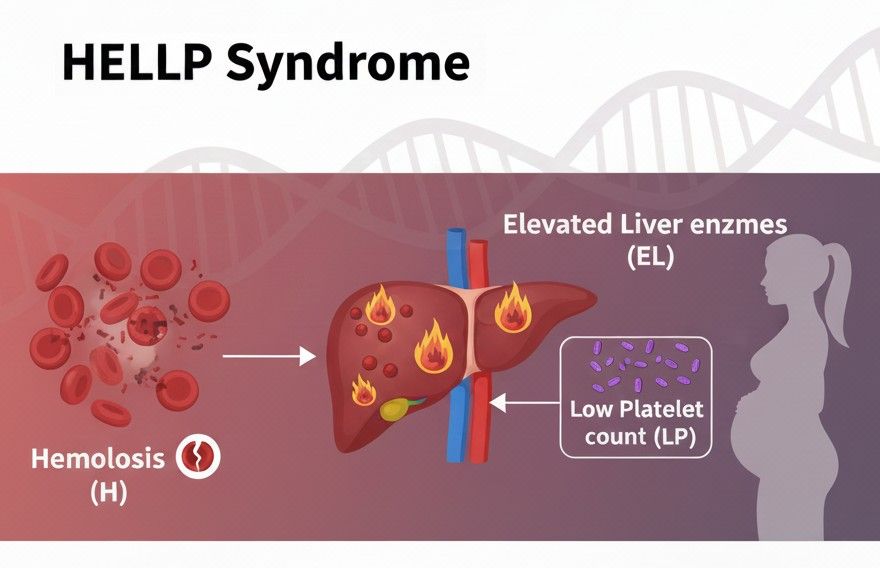
HELLP Syndrome is a severe and potentially life-threatening pregnancy complication that usually occurs in the later stages of pregnancy or shortly after childbirth. The name HELLP is an acronym that stands for:
- H – Hemolysis (breakdown of red blood cells)
- EL – Elevated Liver enzymes (indicating liver damage)
- LP – Low Platelet count (which affects blood clotting)
In simple words, HELLP Syndrome affects the blood and the liver simultaneously. It disrupts the body’s ability to properly carry oxygen, damages liver function, and reduces the blood’s ability to clot. If not treated immediately, it can cause serious harm to both the mother and the baby.
HELLP is often considered a complication of preeclampsia, a condition marked by high blood pressure during pregnancy. However, what makes HELLP particularly dangerous is that it can develop even without obvious signs of high blood pressure.
This is why doctors call it one of the most unpredictable and dangerous complications of pregnancy.
Causes of HELLP Syndrome
The exact cause of HELLP Syndrome is still not completely understood, which makes it even more frightening. However, doctors and researchers believe it develops due to abnormal changes in the placenta and blood vessels during pregnancy, leading to widespread damage in the mother’s body. Here are the main factors believed to cause HELLP Syndrome:
Abnormal Placental Development
In a healthy pregnancy, the placenta allows oxygen and nutrients to flow smoothly from mother to baby. In HELLP syndrome, the blood vessels that supply the placenta do not form or function properly. This leads to reduced blood flow, which triggers damage to blood and liver cells.
Severe Preeclampsia
HELLP is considered a life-threatening form of preeclampsia. High blood pressure can damage blood vessels, causing red blood cells to break apart and affecting the liver and clotting system.
Damage to Blood Vessels
The inner lining of blood vessels becomes injured, causing platelets to be used up rapidly and red blood cells to break down. This is what leads to low platelets and hemolysis.
Immune System Response
In some women, the immune system may react abnormally to the pregnancy. This exaggerated inflammatory response can harm the liver and interfere with normal blood clotting.
Genetic Factors
HELLP Syndrome sometimes runs in families. A genetic predisposition may make certain women more susceptible to developing it, especially if their mother or sister had it.
Liver Stress and Dysfunction
As the condition progresses, the liver becomes inflamed and stressed. Liver cells are damaged, causing liver enzymes to rise sharply. In severe cases, bleeding can occur inside the liver.
Hormonal Imbalances
Sudden or intense hormone changes during late pregnancy can affect the way the blood and vessels respond, possibly increasing the risk of HELLP.
Placental Abruption
HELLP Syndrome may develop alongside placental abruption, where the placenta separates too early from the uterus. This causes heavy bleeding and worsens complicati
Who is at Risk of HELLP Syndrome?
While HELLP Syndrome can affect any pregnant woman, certain factors increase the risk:
- Women with preeclampsia or eclampsia
- First-time mothers
- Women over the age of 35
- Women with a history of HELLP in a previous pregnancy
- Those carrying twins or multiples
- Women with pre-existing conditions like diabetes or high blood pressure
- Obesity or poor nutritional status
- Family history of pregnancy complications
- Kidney disease
- Autoimmune conditions such as lupus
But here’s the truth: HELLP can still occur in completely healthy women with normal pregnancies. That’s what makes awareness so much more important. It can happen to anyone, and often without clear warning signs.
Why HELLP Syndrome is So Dangerous
One of the scariest aspects of HELLP Syndrome is how quickly it can progress. A woman might feel mostly fine in the morning and be critically ill by night.
The condition can lead to:
- Liver rupture
- Severe internal bleeding
- Stroke
- Kidney failure
- Placental abruption (when the placenta separates from the uterus)
- Preterm birth
- Stillbirth
Without prompt medical intervention, HELLP Syndrome can be fatal.
Yet, with timely diagnosis and proper care, many mothers and babies survive and recover well. The key is rapid recognition and immediate treatment.
Symptoms of HELLP Syndrome
This is where HELLP becomes tricky. Its symptoms can be mistaken for everyday pregnancy discomforts, stress, flu, or indigestion.
Some of the most common symptoms include:
- Severe headache that does not go away
- Blurred vision or sensitivity to light
- Upper right abdominal pain (especially under the ribs)
- Shoulder or back pain
- Nausea and vomiting (especially in the third trimester)
- Sudden, intense fatigue
- Swelling in the face and hands
- Rapid weight gain due to fluid retention
- Nosebleeds or easy bruising
- Difficulty breathing
- Feeling generally unwell or anxious
Many women describe it not as sharp pain, but as a deep, crushing discomfort in the upper abdomen. Some think it’s food poisoning or heartburn. Others believe it’s just a tough pregnancy day.
And that’s the danger.
If you ever feel that something isn’t right during pregnancy, trust your instincts and seek medical attention immediately.
How is HELLP Syndrome Diagnosed?
HELLP is diagnosed through blood tests and clinical observations. The doctor will typically order:
- A complete blood count to check platelet levels
- Liver function tests to measure enzymes
- Tests to detect hemolysis (red blood cell breakdown)
- Urine tests to check protein levels
- Blood pressure monitoring
- Ultrasound or CT scan if liver complications are suspected
The diagnosis is usually based on these three findings:
- Evidence of hemolysis
- Elevated liver enzyme levels
- Low platelet count
In some cases, HELLP is divided into classes based on platelet count severity. This helps doctors determine the urgency and treatment plan.
Once HELLP is suspected or confirmed, the situation becomes a medical emergency.
Treatments for HELLP Syndrome
There is no “cure” for HELLP Syndrome apart from delivering the baby. That’s a hard truth, and for women who are still early in their pregnancy, it can be heartbreaking.
The goal of treatment is to:
- Stabilize the mother
- Prevent complications
- Prepare the baby for birth (if preterm)
- Deliver safely as soon as possible
Treatment may include:
- Hospitalization in an intensive care unit
- Medications to lower blood pressure
- Corticosteroids to improve the baby’s lung development
- Magnesium sulfate to prevent seizures
- Blood or platelet transfusions
- Emergency cesarean section in severe cases
In milder cases close to full-term, doctors may try to delay delivery for a short time to strengthen the baby’s lungs. But in most cases, delivery happens within 24 to 48 hours of diagnosis.
The safety of the mother is always the top priority.
HELLP Syndrome After Delivery
Many people believe that once the baby is born, everything will go back to normal quickly. But with HELLP Syndrome, this is not always true.
In fact, HELLP often worsens in the first 24–48 hours after delivery before it starts improving. This is why close monitoring is crucial even after childbirth.
Mothers may still experience:
- High blood pressure
- Fatigue
- Emotional distress
- Pain and weakness
- Need for blood transfusions
- Extended hospital stay
The recovery period can be physically and emotionally draining. Some women need weeks, or even months, to feel normal again.
And while everyone is celebrating the newborn, the mother is still healing from a life-threatening condition.
This is why emotional support is just as important as medical care.
Can You Have HELLP Syndrome Again?
One of the biggest fears for women who’ve experienced HELLP is: Will it happen again?
The answer is: it’s possible, but not guaranteed.
Studies show that the risk of recurrence ranges between 5% and 25%, depending on factors like severity and underlying conditions.
If you’ve had HELLP before, your pregnancy will be considered high-risk, and your doctor will monitor you very closely in future pregnancies. Early prenatal care, regular blood tests, and vigilant monitoring can help catch warning signs early. Many women go on to have healthy, normal pregnancies after HELLP.
Impact on the Baby
The baby is affected mostly due to premature birth and reduced oxygen supply caused by placental problems.
Possible risks include:
- Low birth weight
- Breathing problems
- Feeding difficulties
- Developmental delays in severe cases
- Need for NICU care
However, medical advancements have significantly improved survival rates and outcomes for premature babies. With proper neonatal care, many babies born during HELLP pregnancies grow up healthy and strong.
And for many mothers, that first cry in the delivery room becomes the moment they realize they survived something unimaginable.
Emotional and Psychological Impact
Not many people talk about the mental and emotional scars left by HELP Syndrome.
After such a traumatic experience, it is common for women to feel:
- Anxiety about future pregnancies
- Postpartum depression
- Post-traumatic stress
- Fear and guilt
- Detachment from their own body
- Confusion about what even happened
HELLP Syndrome can happen so suddenly that women barely have time to process it.
One moment they are preparing a nursery, and the next they are in an operating room signing emergency forms for survival.
Healing from HELLP is not just physical. It’s emotional and psychological too.
Talking about it, joining support groups, and seeking therapy can be extremely healing.
How to Reduce the Risk of HELLP Syndrome
While HELLP cannot always be prevented, you can reduce your risk by:
- Attending all prenatal check-ups
- Monitoring your blood pressure regularly
- Reporting any unusual symptoms immediately
- Eating a balanced and nutritious diet
- Staying properly hydrated
- Managing stress levels
- Avoiding smoking and alcohol
- Managing chronic illnesses under medical supervision
Listening to your body is the most powerful tool you have.
Never ignore persistent pain, strange discomfort, or a feeling that something is wrong. You know your body better than anyone else.
HELLP Syndrome vs Preeclampsia
While HELLP is related to preeclampsia, it is more dangerous and complex.
| Preeclampsia | HELLP Syndrome |
|---|---|
| Mainly involves high blood pressure | Involves blood and liver damage |
| Develops slowly | Can progress rapidly |
| Usually diagnosed through BP and urine tests | Diagnosed through blood tests |
| Moderate to severe | Always considered severe |
| May be managed longer | Requires urgent treatment |
Some women develop HELLP without ever having noticeable preeclampsia symptoms.
This is why doctors emphasize blood tests when women complain of certain symptoms in late pregnancy.
Real-Life Reality: What a HELLP Experience Feels Like
Many women who have gone through HELLP describe it in similar words:
“I felt like something was tearing me from the inside.”
“I thought it was just heartburn, but it was much worse.”
“I was scared but too tired to even cry.”
“One minute I was fine, the next I was fighting for my life.”
“I never imagined pregnancy could turn into this.”
It’s not just a medical condition. It is a survival story for many women.
HELLP Syndrome takes away the picture-perfect image of pregnancy and replaces it with fear, strength, and resilience.
Life After HELLP Syndrome
Recovery is not linear. Some days you will feel strong. Some days you will feel broken.
But slowly, healing happens.
Your blood levels return to normal. Your strength comes back. Your scars, both visible and invisible, begin to soften.
And then one day, you look at your child and realize: you made it.
You survived HELLP Syndrome.
Life after HELLP is about:
- Prioritizing your health
- Honoring your strength
- Sharing your story
- Advocating for awareness
- Living with gratitude
Final Thoughts
HELLP Syndrome may be rare, but it is dangerously real. It does not care who you are, how healthy you are, or how perfect your pregnancy seems.
That’s why it’s vital to talk about it — to raise awareness and to help women recognize the signs early.
- If you are pregnant, never ignore unusual symptoms.
- If your friend is pregnant, share this knowledge.
- If you survived HELLP, your story matters.
Because awareness can save a life.
FAQ’s
How common is HELLP Syndrome?
HELLP Syndrome is considered rare, affecting about 1–2 out of every 1,000 pregnancies. However, among women with severe preeclampsia, the risk is much higher.
Can HELLP Syndrome occur without high blood pressure?
Yes, HELLP Syndrome can develop even in women who do not have noticeable high blood pressure. This is what makes it especially dangerous, as it may go undetected at first.
What are the first warning signs of HELLP Syndrome?
Common early symptoms include severe headache, nausea and vomiting, upper right abdominal pain, vision issues, swelling in the face or hands, extreme fatigue, and a general feeling that something is wrong.
Is HELLP Syndrome dangerous for the baby?
Yes, HELLP Syndrome can reduce blood flow to the baby and often leads to premature delivery. This can cause low birth weight and the need for neonatal intensive care, but many babies do well with proper medical support.
Can HELLP Syndrome be treated without delivering the baby?
In most cases, delivering the baby is the only effective way to stop HELLP Syndrome from progressing. Doctors may delay delivery for a short time if it is safe, to help the baby’s lungs mature.
How long does it take to recover from HELLP Syndrome?
Physical recovery can take several weeks, and full emotional recovery may take longer. Blood and liver levels usually begin to normalize within days after delivery, but fatigue and weakness can persist.
Can HELLP Syndrome come back in another pregnancy?
Yes, there is a risk of recurrence, but it is not guaranteed. The estimated risk is between 5% and 25%. With close monitoring and early care, many women go on to have healthy pregnancies.
Is HELLP Syndrome the same as preeclampsia?
No, but it is closely related. Preeclampsia mainly causes high blood pressure and protein in the urine, while HELLP Syndrome affects the blood, liver, and platelets and is usually more severe.
What should I do if I suspect HELLP Syndrome?
Seek immediate medical attention. Go to the nearest hospital or contact your doctor as soon as possible. Early intervention can be life-saving for both mother and baby.
Is there life after HELLP Syndrome?
Absolutely. With proper medical care, emotional support, and time to heal, most women recover and go on to live healthy lives and even have successful future pregnancies.
What is the role of MgSO₄ in HELLP syndrome?
Magnesium sulfate (MgSO₄) is given to prevent seizures in women with HELLP syndrome. It helps calm the nervous system and lowers the risk of serious complications like eclampsia, but it does not cure the condition.
What is the emergency management of HELLP syndrome?
Emergency treatment includes immediate hospitalization, blood pressure control, magnesium sulfate to prevent seizures, possible blood transfusions, and urgent delivery of the baby, which is the only definitive treatment for HELLP syndrome.
Also Read: