Cancer treatment has evolved tremendously over the years, from traditional chemotherapy and radiation to targeted therapies and immunotherapy. Among these advancements, CAR T-cell therapy has emerged as a groundbreaking approach, offering hope to patients with difficult-to-treat cancers. This innovative technique harnesses the power of the body’s immune system to specifically target and eliminate cancer cells.
Could CAR T-cell therapy be the future of cancer treatment? Let’s explore how it works, its benefits, challenges, and its potential to change the medical landscape.
What is CAR T-Cell Therapy?
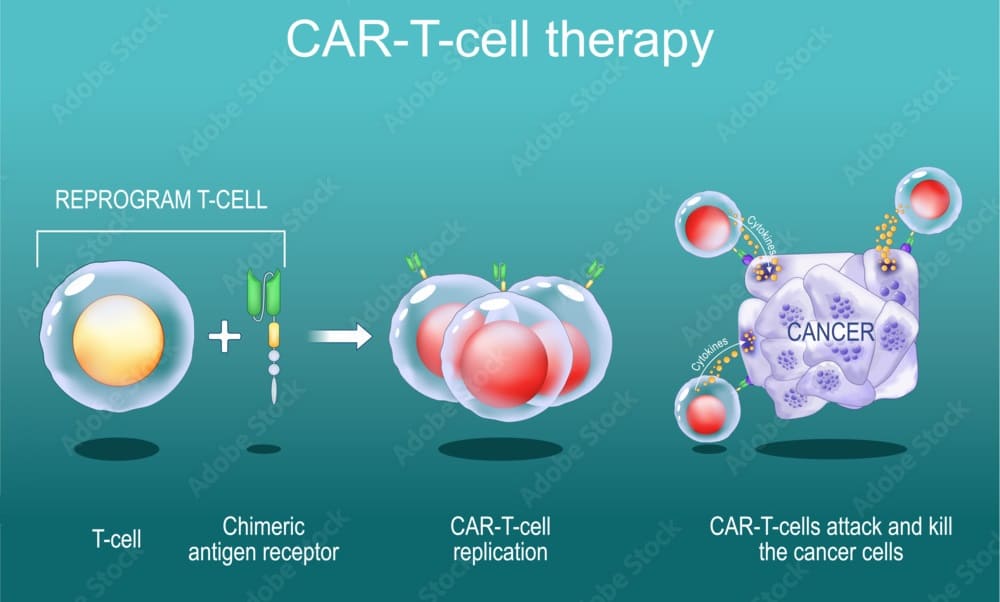
Chimeric Antigen Receptor (CAR) T-cell therapy is a personalized cancer treatment that involves genetically modifying a patient’s immune cells (T cells) to recognize and attack cancer cells. T cells are a type of white blood cell that play a crucial role in the immune system by identifying and destroying infected or abnormal cells. However, cancer cells often evade detection by disguising themselves as normal cells.
CAR T-cell therapy enhances the T cells’ ability to recognize cancer cells by equipping them with a special receptor—the chimeric antigen receptor (CAR)—that specifically targets proteins found on cancer cells. Once infused back into the patient’s body, these engineered T cells become powerful cancer fighters.
How Does CAR T-Cell Therapy Work?
The treatment process involves multiple steps, requiring advanced genetic engineering and laboratory techniques. Here’s a step-by-step breakdown:
1) T-Cell Collection (Apheresis):
Doctors extract T cells from the patient’s blood through a process called apheresis. This is similar to donating blood but focuses on collecting specific immune cells while returning the remaining blood components to the patient.
2) Genetic Modification in the Lab:
In a specialized laboratory, scientists modify the extracted T cells by inserting a gene that encodes the chimeric antigen receptor (CAR). This receptor allows the T cells to detect and attack cancer cells more effectively.
3) Cell Multiplication:
The newly engineered T cells are then grown and multiplied in large numbers to ensure there are enough to fight the cancer effectively. This process can take several weeks.
4) Pre-Treatment (Lymphodepleting Chemotherapy):
Before reinfusing the modified T cells, the patient undergoes lymphodepleting chemotherapy to temporarily suppress the immune system. This creates a more favorable environment for the infused CAR T cells to expand and function effectively.
5) Infusion of CAR T Cells:
The modified T cells are infused back into the patient’s bloodstream through an intravenous (IV) drip. Once inside, these cells seek out and destroy cancer cells that express the specific target antigen.
6) Cancer Attack and Immune Memory:
Once inside the body, CAR T cells act like “living drugs,” continuously patrolling for cancer cells. Unlike traditional treatments that require repeated cycles, CAR T cells can remain active for years, providing long-term protection and potential remission.
Why is CAR T-Cell Therapy a Game Changer?
CAR T-cell therapy represents a paradigm shift in cancer treatment, offering benefits that traditional therapies cannot match:
1) Highly Targeted Treatment:
Unlike chemotherapy and radiation, which damage both cancerous and healthy cells, CAR T-cell therapy specifically targets cancer cells, minimizing harm to normal tissues.
2) Long-Lasting Effects:
Unlike conventional treatments that require continuous administration, CAR T cells persist in the body long after infusion, providing ongoing surveillance against cancer recurrence.
3) High Success Rates in Blood Cancers:
CAR T-cell therapy has shown remarkable success in treating certain blood cancers, including:
- Acute lymphoblastic leukemia (ALL)
- Diffuse large B-cell lymphoma (DLBCL)
- Multiple myeloma
Many patients who had exhausted all other treatment options achieved complete remission with CAR T-cell therapy.
Current Challenges and Limitations
While CAR T-cell therapy offers hope, it is not without challenges:
1) High Cost and Limited Accessibility:
CAR T-cell therapy is one of the most expensive cancer treatments, costing $350,000–$500,000 per patient in the U.S. Efforts are being made to reduce costs and expand access worldwide.
2) Severe Side Effects:
Some patients experience Cytokine Release Syndrome (CRS), a life-threatening immune reaction that can cause:
- High fever
- Low blood pressure
- Organ failure
Another potential side effect is Neurotoxicity, which can cause confusion, seizures, or difficulty speaking. However, medical advancements are improving management strategies for these risks.
3) Limited Success in Solid Tumors:
CAR T-cell therapy has shown tremendous success in blood cancers but faces challenges in treating solid tumors like lung, breast, or colon cancer. Scientists are working on improving CAR T-cell therapy for these cancers by:
- Enhancing T cell penetration into tumors
- Overcoming the tumor’s protective environment
- Finding new antigen targets
The Future of CAR T-Cell Therapy
Despite these challenges, CAR T-cell therapy is rapidly evolving. Researchers are exploring next-generation CAR T-cell therapies that:
- Target multiple antigens to prevent cancer resistance
- Use gene-editing tools like CRISPR to enhance T cell effectiveness
- Expand to treat autoimmune diseases and solid tumors
Several clinical trials are underway to make CAR T-cell therapy safer, more effective, and accessible to more patients.
Is CAR T-Cell Therapy the Future of Cancer Treatment?
CAR T-cell therapy is one of the most promising breakthroughs in cancer treatment, offering long-lasting remission and hope to patients who had no other options. While challenges remain, ongoing research and technological advancements could make this therapy more accessible and effective for a wider range of cancers.
As scientists continue refining CAR T-cell therapy, we may be on the brink of a revolution in cancer treatment—one where a patient’s own immune system becomes the ultimate weapon against cancer.
Also Read: